A rare case of hematologic peritonitis complicating secondary myelofibrosis
DOI:
https://doi.org/10.25796/bdd.v8i3.87085Keywords:
peritoneal dialysis, peritonitis, cloudy peritoneal dialysate, culture-negative peritonitis, secondary myelofibrosisAbstract
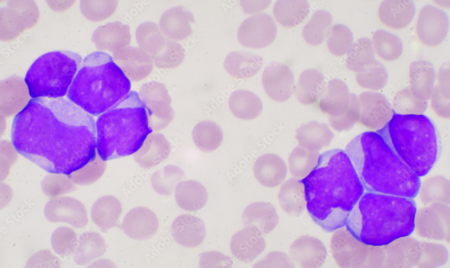
Peritonitis is a frequent complication of peritoneal dialysis. Its diagnosis is based on clinical signs (pain, cloudy effluent), intraperitoneal hyperleukocytosis (> 0.1×109/L with more than 50% polynuclears), or a positive culture. Although the majority of peritonitis cases are of infectious origin, there are also cases due to non infectious origin, which can lead to the inappropriate use of antibiotics and delayed diagnosis. We report the case of a 78-year-old male patient with a complex haemopathy that combined paroxysmal nocturnal haemoglobinuria, despite treatment with ravulizumab, and essential thrombocythemia, which transformed into myelofibrosis. After the initiation of peritoneal dialysis treatment, he presented with occasionally cloudy dialysis fluid rich in leukocytes (up to 0.442 ×10^9/L), with no evidence of infection (negative cultures and DNA16S PCR, moderate CRP, and an absence of atypical cells). The origin of the intraperitoneal hyperleukocytosis was attributed to myelofibrosis-related blood hyperleukocytosis. The clinical course was unfavorable, leading to palliative management.
This case illustrates the difficulty of managing this complication in peritoneal dialysis patients. Although infectious peritonitis is the most common first-line diagnosis, it is important to consider various differential diagnoses in cases of culture-negative peritonitis, particularly hematological causes (leukemia, lymphoma, myelofibrosis). However, forms with a predominance of neutrophils in the dialysate may simulate an infection. The absence of fever, elevated CRP, and a correlation between blood and peritoneal hyperleukocytosis should help in making a differential diagnosis. Immunophenotyping or molecular biology in the dialysate could refine the diagnosis. This case highlights a possible cause of sterile peritonitis due to myelofibrosis with hyperleukocytosis, and calls for recommendations to be adapted to increasingly complex clinical situations.
INTRODUCTION
Peritoneal dialysis is one of the techniques used for renal replacement therapy. It is commonly used in France, although much less than hemodialysis [1]. Like any technique, it is not without complications, the most well-known of which is peritonitis [2][3].
The diagnosis of peritonitis is based on the presence of at least two of the following [4]:
- clinical features consistent with peritonitis, i.e., abdominal pain or cloudy dialysis effluent;
- a white blood cell count in dialysis effluent > 100/µL or > 0.1 × 109/L (after a stasis time of at least 2 hours), with > 50% polymorphonuclear leukocytes (PMNs);
- a positive culture in the dialysis effluent.
The majority of peritonitis cases are infectious in origin, but other etiologies must be considered and investigated [5][6][7][8]. Signs of peritonitis are usually interpreted as infectious in origin to avoid delays in treatment, which can lead to significant morbidity and mortality. However, this can lead to complications, including the excessive use of antibiotics, which risks altering the bacterial ecology and promoting antibiotic resistance; it can also lead to delayed management of the underlying disease (which may be iatrogenic, an allergy, an oncological or hematological condition, or a surgical pathology). The recommendations for managing peritonitis [[4]] emphasize the need to initiate antibiotics promptly, given the potential severity of the infection; however, this recommendation must be qualified, and management must be adapted on a case-by-case basis.
Nephrology patients are often elderly, have multiple pathologies, and are on multiple medications. This presents us with a complex pattern of complications and observations, particularly in oncological and hematological contexts.
We report here a case of non-infectious peritonitis manifesting as sometimes cloudy peritoneal dialysis effluent, associated with an excess of intraperitoneal white blood cells secondary to blood hyperleukocytosis, itself a consequence of a hematological disease.
CASE PRESENTATION
A 78-year-old man developed stage V chronic kidney disease in the context of paroxysmal nocturnal hemoglobinuria that progressed despite treatment with ravulizumab (Ultomiris®, Alexion Pharma France) and then eculizumab (Soliris®, Alexion Pharma France). He had a history of paroxysmal nocturnal hemoglobinuria and also essential thrombocythemia with a cytogenetic diagnosis of MPL W515L and associated DNMT3A mutation, which secondarily transformed into myelofibrosis and had been treated with hydroxyurea (Hydrea®) and ruxolitinib (Jakavi®) since 2023 (with known hyperleukocytosis at 30G/L). He also presented with flutter and high blood pressure.
He began emergency extrarenal purification by hemodialysis after placement of a right internal jugular tunneled catheter on October 28, 2024, followed by peritoneal dialysis on January 6, 2025 (after placement of a peritoneal dialysis catheter accompanied by treatment for an inguinal hernia on December 9, 2024). His protocol included a short exchange (4 hours) of isotonic solution (Physioneal 40® with 1.36% glucose, Baxter International Inc.) and a long exchange of hypertonic solution (Extraneal®, Baxter International Inc.) for the rest of the nycthemeral cycle. The protocol was adapted to the patient's needs, his residual renal function, and the availability of registered nurses.
On January 13, 2025, his nurses reported difficulty with drainage and that the patient was suffering from abdominal pain. He was admitted to the day hospital and underwent an exchange, which restored the drainage fluid to a clear state. However, cytological examination revealed a white blood cell count of 0.139 × 109/L, with 53% polynuclear cells. Blood tests showed a CRP of 8 mg/L, a hemoglobin level of 9 g/dL, and a white blood cell count of 63 × 109/L, with 36 × 109/L of polynuclear cells.
Bacteriological samples of dialysis fluid and blood were cultured. The ASP found the catheter in place but with an accumulation of fecal matter. Because of the possibility of infectious peritonitis related to peritoneal dialysis, he was given empirical intraperitoneal antibiotic treatment with cefazolin and ceftazidime (in accordance with the Toulouse University Hospital protocol). Given his stable clinical condition, the patient was discharged home.
On January 14, 2025, he was re-evaluated in consultation due to persistent abdominal pain and slightly cloudy drainage fluid. Cytological examination revealed an elevated white blood cell count of 0.197 × 109/L, with 51% polymorphonuclear cells. He was admitted to the nephrology department on the same day.
Physical examination on admission showed no fever, a blood pressure of 160/80, and a heart rate of 70 bpm. Cardiopulmonary auscultation was normal. The abdomen was tender with no guarding or contracture. The results of laboratory and imaging tests after admission were as follows:
-Cytological analysis of the dialysis fluid revealed a white blood cell count of 0.201 × 109/L, with 29 % polynuclear cells.
- The effluent culture was negative, as was the 16S DNA (bacterial DNA by PCR),
-Blood te sts revealed a CRP of 4.4 mg/L, a hemoglobin level of 8.7 g/dL, and a white blood cell count of 67 × 109/L with a predominance of PNN.
-All blood cultures were negative.
-Computed tomography revealed parietal thickening of the colon associated with infiltration of peritoneal fat.
Given the results and despite no increase in CRP, a diagnosis of colitis without peritonitis was made, prompting a change in antibiotic therapy to intravenous tazocillin for a total duration of 7 days. The patient was discharged home.
On February 3, due to persistent asthenia, tests were performed to assess the progression of the patient's hematological disease:
-A myelogram showed poor bone marrow with hypoplasia of the erythroid lineage and moderate dysmyelopoiesis, without excess blasts.
-Lymphocyte phenotyping of the bone marrow showed no significant expansion of lymphocyte subpopulations.
-Molecular biology analysis to detect hematological disorders revealed the previously described DNMT3A mutation.
On February 5, 2025, the patient was hospitalized due to a deterioration in his general condition and spontaneous bleeding. Physical examination on admission showed a blood pressure of 130/60 and a heart rate of 70 bpm, with no fever. Cardiopulmonary auscultation was normal. The abdomen was still tender.
Drainage of PD fluid revealed it to be cloudy without fibrin. Analysis of the fluid showed a white blood cell count of 0.442 × 109/L, with 41% polynuclear cells. Blood tests revealed a CRP of 2.9 mg/L, a hemoglobin level of 10.2 g/dL, and a white blood cell count of 62 × 109/L (Table I). All cultures were negative.
| Date | Effluent appearance | Blood WBC (x109 /L) | CRP (mg/L) |
Effluent WBC (x109 /L) |
Effluent Neutrophils (in %) |
Effluent Basophils (in %) |
Effluent Lymphocytes (in %) |
Effluent Monocytes (in %) |
|---|---|---|---|---|---|---|---|---|
| 13/01/2025 | Clear | 63 | 8 | 0.139 | 53 | 1 | 2 | 44 |
| 14/01/2025 | Cloudy | NA | NA | 0.197 | 51 | 1 | 3 | 45 |
| 15/01/2025 | Cloudy | 67 | 4.4 | 0.201 | 2 | 1 | 7 | 63 |
| 05/02/2025 | Cloudy | 62 | 2.9 | 0.442 | 41 | 1 | 2 | 56 |
It should be noted that none of the dialysis fluid analyses revealed any atypical cells on the slides examined. We did not perform phenotyping of the dialysis effluent, as phenotyping of the bone marrow was normal.
The diagnosis was terminal hematological disease with intraperitoneal hyperleukocytosis secondary to blood hyperleukocytosis refractory to medical treatment. However, this remains a hypothesis since we did not perform molecular biology analysis on the effluent, which would have allowed us to confirm the presence of pathological cells associated with the previously described mutation. The prognosis was poor, and the patient was shifted toward palliative care.
DISCUSSION
Infectious peritonitis during peritoneal dialysis is a classic complication with an initially low morbidity and mortality rate, which increases significantly if treatment is delayed. Peritoneal infections are a fairly common reason for discontinuing peritoneal dialysis and switching to hemodialysis. In 2018, according to the RDPLF, 14% of such transfers were secondary to peritonitis [9].
In addition, sterile peritonitis is a common problem in patients receiving peritoneal dialysis. It is, therefore, essential to be able to diagnose and manage the various causes of peritonitis.
Previous studies found peritoneal dialysate cultures to be negative in 20% of cases [10], but more recent work has found negative cultures in between 10 and 15% of cases (14.6% according to the RDPLF in 2017, and 13.7% at Toulouse University Hospital between January 1, 2020, and January 1, 2025). In these situations, it is essential first to rule out an infectious cause that is difficult to identify, such as mycobacteria, fungi, or parasites. It is then useful to look at the distribution of different types of cells in the dialysate sample. When the sample is predominantly composed of neutrophils, the possibility of infectious peritonitis remains, and it is sometimes difficult to justify continuing antibiotic therapy in cases of culture-negative infectious peritonitis.
However, when the white blood cells are predominantly neutrophils and an infectious cause cannot be determined, it is necessary to look for other etiologies [8], such as:
- Inflammation of intraperitoneal organs (appendicitis, cholecystitis, etc.),
- Inflammation of retroperitoneal organs (such as splenic infarction, splenic abscess, or pancreatitis) [11][12][13][14][15],
-Malignant tumors of solid organs (such as renal carcinomas or endometrial cancer) [16][17][18][19].
After reviewing the literature, we created a table (Table II) of possible etiologies of neutrophil-predominant leukocytosis in peritoneal dialysis fluid with a sterile culture.
Table II. Possible causes of neutrophilic leukocytosis with sterile peritoneal dialysis fluid.
| CATEGORY | ETIOLOGIES | PROPOSALS |
|---|---|---|
| Actual infection but negative culture | Mycobacteria (TB)Fungi (Candida, Aspergillus, Mucormycosis)Fastidious bacteria (Brucella, Legionella)Poor sampling of anaerobes | Germs that are difficult to isolate: prolonged cultures or PCR often necessary |
| Prior antibiotic therapy | Antibiotics started before sampling | Antibiotic therapy window to be discussed |
| Technical error | Inadequate sampling or transportContamination of the vial | Repeat sampling |
| Chemical peritonitis | Irritation from antiseptic (iodine, chlorhexidine)Rupture of the dialysis bag | |
| Hemoperitoneum | Secondary trauma to the catheter with digestive perforation | Imaging+/- endoscopy+/- surgical management |
| Inflammatory or autoimmune disease | Systemic lupus erythematosusVasculitis | |
| Inflammation of the intraperitoneal organs | AppendicitisCholecystitis | Imaging |
| Inflammation of the retroperitoneal organs | Acute pancreatitisSplenic abscessSplenic infarction | ImagingBiology (including lipase/amylase) |
| Malignant tumor of solid organs/peritoneal carcinomatosis | Renal carcinomasEndometrial cancerPeritoneal metastasesLymphoma | Imaging+/- biopsy or excision+/- PD effluent analysis in anatomopathology, immunophenotyping, molecular biology |
| Hollow organ rupture | Perforated ulcer, diverticulitis, appendicitis | Imaging+/- surgical management |
| Ischemia | Mesenteric ischemia (AMS occlusion) | Imaging |
Hematological causes are mainly found when the dialysis fluid is predominantly lymphocytic, with lymphoma being the most common etiology. After reviewing the literature, we found six reported cases of lymphoma diagnosed in the context of suspected peritonitis [20][21][22][23][24][25]. The pathophysiological explanation is the presence of an increased number of atypical lymphocytes secondary to intraperitoneal diffusion. It is, therefore, possible that other hematological diseases may be complicated by aseptic peritonitis. However, we have not found any other cases in the current literature.
Essential thrombocythemia can, in some cases, develop into secondary myelofibrosis. The complications of secondary myelofibrosis can be divided into three groups:
- General signs including asthenia, sweating, and hyperthermia,
- Myeloproliferation, including splenomegaly and hyperleukocytosis,
- Cytopenias, including anemia and thrombocytopenia.
These complications develop at varying rates and can therefore sometimes mimic infections (particularly hyperthermia and hyperleukocytosis). In some cases, significant hyperleukocytosis is present, which is a marker of poor prognosis with a risk of resistance to ruxolitinib and unfavorable disease progression [26].
In this clinical case, we collected clinical and biological data from a patient who presented with sterile peritonitis during peritoneal dialysis. The data suggested that this peritonitis was secondary to his hematological disease, namely essential thrombocythemia with secondary myelofibrosis.
In this clinical case, we collected clinical and biological data from a patient who presented with sterile peritonitis during peritoneal dialysis. The data suggested that this peritonitis was secondary to his hematological disease, namely essential thrombocythemia with secondary myelofibrosis. However, this case shows the limitations of such a diagnosis as a first-line approach. Indeed, it is difficult not to consider infectious peritonitis when intraperitoneal leukocytes are present above the threshold considered pathological and when the percentage of neutrophils is greater than 50%. Moreover, the initial observation of the case may have been related to a digestive infection, an initial flare-up of the patient's hematological disease, or a combination of the two. It is difficult to choose between the two hypotheses. We observed that the dialysis fluid became more mixed than it was initially, which points toward a hematological cause.
When hematological peritonitis is suspected, it may be useful to perform lymphocyte immunophenotyping or molecular biology analysis of the dialysis effluent, depending on the suspected cause and diagnostic method. This could have helped us confirm the diagnosis of hematological peritonitis.
These results show that certain clinical and biological markers should alert us to seek differential diagnoses for infectious peritonitis, particularly apyrexia and the absence of associated biological inflammatory syndrome (CRP). In addition, they highlight a new possible cause of culture-negative peritonitis.
CONCLUSION
This observation highlights a new alternative diagnosis for sterile peritonitis, encouraging the consideration of new causes of culture-negative peritonitis. Nevertheless, physicians should remain vigilant for infectious peritonitis, which should be considered as the primary diagnosis.
Author contributions
ChG contributed to data collection and analysis, study design and methodology, and the writing of the original manuscript. HEH reviewed the literature and revised the manuscript. ClG and MBN performed the final review and approved the manuscript for publication.
Ethical statement
In accordance with ethical requirements, we specify that informed consent could not be obtained, as the study was conducted retrospectively after the patient's death.
Funding
The authors received no financial support for the research, writing, or publication of this article.
Conflicts of interest
No conflicts of interest to declare.
ORCIDids
Charlotte Gabilan : https://orcid.org/0009-0002-5048-7657
Marie Béatrice Nogier : https://orcid.org/0000-0001-9888-2547
References
- Réseau R.E.I.N.. Synthèse du rapport annuel 2022 du réseau REIN.Publisher Full Text
- Sahlawi Muthana Al. Peritoneal dialysis-associated peritonitis outcomes reported in trials and observational studies: A systematic review. Peritoneal dialysis international: journal of the International Society for Peritoneal Dialysis. 2020; 40,2:132-140. DOI
- Marshall Mark R.. A systematic review of peritoneal dialysis-related peritonitis rates over time from national or regional population-based registries and databases. Peritoneal dialysis international: journal of the International Society for Peritoneal Dialysis. 2022; 42,1:39-47. DOI
- Li Philip Kam-Tao. ISPD peritonitis guideline recommendations: 2022 update on prevention and treatment. Peritoneal dialysis international: journal of the International Society for Peritoneal Dialysis. 2022; 42,2:110-153. DOI
- Verger C., Veniez G., Dratwa M.. Variability of aseptic peritonitis rates in the RDPLF.DOI
- Rocklin M.A., Teitelbaum I.. Noninfectious causes of cloudy peritoneal dialysate. Seminars in dialysis. 2001; 14,1:37-40. DOI
- Teitelbaum Isaac. Cloudy peritoneal dialysate: it’s not always infection. Contributions to nephrology. 2006; 150:187-194. DOI
- Cheng Xin Bo Justin, Bargman Joanne. Complications of Peritoneal Dialysis Part II: Nonmechanical Complications. Clinical journal of the American Society of Nephrology: CJASN. 2024; 19,6:791-799. DOI
- Verger C., Fabre E., Veniez G., Padernoz M.C.. Données statistiques synthétiques du Registre de Dialyse Péritoneale de Langue Française et Hémodialyse à Domicile (RDPLF) en 2018.
- Freitas DGR Gokal. Sterile peritonitis in the peritoneal dialysis patient. Perit Dial Int. 2005;146-51.
- Yang C.C.. Splenic infarction: an unrecognized cause of culture-negative peritonitis in a continuous ambulatory peritoneal dialysis patient. Clinical nephrology. 2007; 68,4:262-5. DOI
- Nandagopal L.. Sterile peritonitis because of splenic infarction in a patient on peritoneal dialysis: an unusual presentation. Peritoneal dialysis international : journal of the International Society for Peritoneal Dialysis. 2013; 33,3:339-40. DOI
- Masaki Chiaki. Splenic abscess diagnosed following relapsing sterile peritonitis in a peritoneal dialysis patient: A case report with literature review. Seminars in dialysis. 2021; 34,3:245-251. DOI
- Manga Farhabanu. Acute pancreatitis in peritoneal dialysis: a case report with literature review. European journal of gastroenterology & hepatology. 2012; 24,1:95-101. DOI
- Osaki Yosuke. Peritoneal dialysis-associated peritonitis, caused by superior mesenteric artery thrombosis with intestinal necrosis: a case report. CEN case reports. 2025; 14,1:1-5. DOI
- Chen Chih-Wei. Intestinal goblet cell carcinoid presenting with recurrent sterile peritonitis in a patient on peritoneal dialysis: a case report. BMC nephrology. 2017; 18,1 62DOI
- Streather C.P.. Carcinoma of the kidney presenting as sterile peritonitis in a patient on continuous ambulatory peritoneal dialysis. Nephron. 1991; 58,1DOI
- Jobson V.W., Adams P.L.. Endometrial carcinoma diagnosed by examination of peritoneal dialysate. Obstetrics and gynecology. 1983; 62,2:264-6.
- Akimoto Tetsu. Peritoneal Dialysis and Malignancy: An Experience With a Patient Complicated by Gastric Carcinoma. Clinical medicine insights. Case reports. 2019; 12 1179547619835176DOI
- Vlahakos D.. Lymphoma-mimicking peritonitis in a patient on continuous ambulatory peritoneal dialysis (CAPD. Peritoneal dialysis international: journal of the International Society for Peritoneal Dialysis. 1990; 10,2:165-7.
- Bargman J.M.. Diagnosis of lymphoma in a continuous ambulatory peritoneal dialysis patient by peritoneal fluid cytology. American journal of kidney diseases: the official journal of the National Kidney Foundation. 1994; 23,5:747-50. DOI
- Delgado-Córdova Margarita. Non-Hodgkin lymphoma mimicking peritonitis in a patient on peritoneal dialysis. Nefrologia : publicacion oficial de la Sociedad Espanola Nefrologia. 2014; 34,5:686-7. DOI
- Viray Paul. Hodgkin’s Lymphoma Diagnosed from Peritoneal Effluent. Peritoneal dialysis international : journal of the International Society for Peritoneal Dialysis. 2016; 36,3:350-1. DOI
- Sriperumbuduri Sriram, Zimmerman Deborah. Cloudy Dialysate as the Initial Presentation for Lymphoma. Case reports in nephrology. 2018; 2018DOI
- Vigil Darlene. Noninfectious Cloudy Peritoneal Effluent in a Peritoneal Dialysis Patient with Mantle Cell Lymphoma. Cureus. 2018; 10,10 e3413DOI
- Vannucchi A.M., Kantarjian H.M., Kiladjian J.J.. A pooled analysis of overall survival in COMFORT-I and COMFORT-II, 2 randomized phase III trials of ruxolitinib for the treatment of myelofibrosis. Haematologica. 2015;1139-45. DOI
References
1. Réseau REIN. Synthèse du rapport annuel 2022 du réseau REIN [en ligne]. 2022 [cité le 1 mai 2025]. Disponible sur : https://www.agence-biomedecine.fr/fr/observatoire-de-la-maladie-renale-chronique/synthese-du-rapport-annuel-2022-du-rein-par-et-pour-les-patients-presentant-une-defaillance-renale-et-leurs-proches
2. Sahlawi, Muthana Al et al. “Peritoneal dialysis-associated peritonitis outcomes reported in trials and observational studies: A systematic review.” Peritoneal dialysis international: journal of the International Society for Peritoneal Dialysis vol. 40,2 (2020): 132-140. doi:10.1177/0896860819893810
3. Marshall, Mark R. “A systematic review of peritoneal dialysis-related peritonitis rates over time from national or regional population-based registries and databases.” Peritoneal dialysis international: journal of the International Society for Peritoneal Dialysis vol. 42,1 (2022): 39-47. doi:10.1177/0896860821996096
4. Li, Philip Kam-Tao et al. “ISPD peritonitis guideline recommendations: 2022 update on prevention and treatment.” Peritoneal dialysis international: journal of the International Society for Peritoneal Dialysis vol. 42,2 (2022): 110-153. doi:10.1177/08968608221080586
5. Verger C, Veniez G, Dratwa M. Variability of aseptic peritonitis rates in the RDPLF. Bull Dial Domic [Internet]. 2018 Jun. 13 [cited 2022 Sep. 5];1(1):9-13. Available from: https://doi.org/10.25796/bdd.v1i1.30
6. Rocklin, M A, and I Teitelbaum. “Noninfectious causes of cloudy peritoneal dialysate.” Seminars in dialysis vol. 14,1 (2001) : 37-40. doi:10.1046/j.1525-139x.2001.00012.x
7. Teitelbaum, Isaac. “Cloudy peritoneal dialysate: it’s not always infection.” Contributions to nephrology vol. 150 (2006): 187-194. doi:10.1159/000093594
8. Cheng, Xin Bo Justin, and Joanne Bargman. “Complications of Peritoneal Dialysis Part II: Nonmechanical Complications.” Clinical journal of the American Society of Nephrology: CJASN vol. 19,6 (2024): 791-799. doi:10.2215/CJN.0000000000000418
9. Verger C, Fabre E, Veniez G, Padernoz MC. Données statistiques synthétiques du Registre de Dialyse Péritoneale de Langue Française et Hémodialyse à Domicile (RDPLF) en 2018. Bull Dial Domic [Internet]. 10avr.2019 [cité 12nov.2020];2(1):1-10.
10. De Freitas DG, Gokal R. Sterile peritonitis in the peritoneal dialysis patient. Perit Dial Int. (2005) : 146-51.
11. Yang, C C et al. “Splenic infarction: an unrecognized cause of culture-negative peritonitis in a continuous ambulatory peritoneal dialysis patient.” Clinical nephrology vol. 68,4 (2007) : 262-5. doi:10.5414/cnp68262
12. Nandagopal, L et al. “Sterile peritonitis because of splenic infarction in a patient on peritoneal dialysis: an unusual presentation.” Peritoneal dialysis international : journal of the International Society for Peritoneal Dialysis vol. 33,3 (2013): 339-40. doi:10.3747/pdi.2012.00139
13. Masaki, Chiaki et al. “Splenic abscess diagnosed following relapsing sterile peritonitis in a peritoneal dialysis patient: A case report with literature review.” Seminars in dialysis vol. 34,3 (2021): 245-251. doi:10.1111/sdi.12953
14. Manga, Farhabanu et al. “Acute pancreatitis in peritoneal dialysis: a case report with literature review.” European journal of gastroenterology & hepatology vol. 24,1 (2012): 95-101. doi:10.1097/MEG.0b013e32834d4bcc
15. Osaki, Yosuke et al. “Peritoneal dialysis-associated peritonitis, caused by superior mesenteric artery thrombosis with intestinal necrosis: a case report.” CEN case reports vol. 14,1 (2025): 1-5. doi:10.1007/s13730-024-00894-y
16. Chen, Chih-Wei et al. “Intestinal goblet cell carcinoid presenting with recurrent sterile peritonitis in a patient on peritoneal dialysis: a case report.” BMC nephrology vol. 18,1 62. (2017) doi:10.1186/s12882-017-0477-x
17. Streather, C P et al. “Carcinoma of the kidney presenting as sterile peritonitis in a patient on continuous ambulatory peritoneal dialysis.” Nephron vol. 58,1 (1991) : 121. doi:10.1159/000186395
18. Jobson, V W, and P L Adams. “Endometrial carcinoma diagnosed by examination of peritoneal dialysate.” Obstetrics and gynecology vol. 62,2 (1983) : 264-6.
19. Akimoto, Tetsu et al. “Peritoneal Dialysis and Malignancy: An Experience With a Patient Complicated by Gastric Carcinoma.” Clinical medicine insights. Case reports vol. 12 1179547619835176. (2019) doi:10.1177/1179547619835176
20. Vlahakos, D et al. “Lymphoma-mimicking peritonitis in a patient on continuous ambulatory peritoneal dialysis (CAPD).” Peritoneal dialysis international: journal of the International Society for Peritoneal Dialysis vol. 10,2 (1990) : 165-7.
21. Bargman, J M et al. “Diagnosis of lymphoma in a continuous ambulatory peritoneal dialysis patient by peritoneal fluid cytology.” American journal of kidney diseases: the official journal of the National Kidney Foundation vol. 23,5 (1994) : : 747-50. doi:10.1016/s0272-6386(12)70289-5
22. Delgado-Córdova, Margarita et al. “Non-Hodgkin lymphoma mimicking peritonitis in a patient on peritoneal dialysis.” Nefrologia : publicacion oficial de la Sociedad Espanola Nefrologia vol. 34,5 (2014): 686-7. doi:10.3265/Nefrologia.pre2014.Apr.12386
23. Viray, Paul et al. “Hodgkin’s Lymphoma Diagnosed from Peritoneal Effluent.” Peritoneal dialysis international : journal of the International Society for Peritoneal Dialysis vol. 36,3 (2016): 350-1. doi:10.3747/pdi.2015.00119
24. Sriperumbuduri, Sriram, and Deborah Zimmerman. “Cloudy Dialysate as the Initial Presentation for Lymphoma.” Case reports in nephrology vol. 2018 2192043. 9 Oct. 2018, doi:10.1155/2018/2192043
25. Vigil, Darlene et al. “Noninfectious Cloudy Peritoneal Effluent in a Peritoneal Dialysis Patient with Mantle Cell Lymphoma.” Cureus vol. 10,10 e3413. (2018) doi:10.7759/cureus.3413
26. Vannucchi AM, Kantarjian HM, Kiladjian JJ, et al. A pooled analysis of overall survival in COMFORT-I and COMFORT-II, 2 randomized phase III trials of ruxolitinib for the treatment of myelofibrosis. Haematologica. (2015) : 1139-45. doi:10.3324/
Downloads
Submitted
Accepted
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Charlotte Gabilan

This work is licensed under a Creative Commons Attribution 4.0 International License.






