Recurrence of inguinal hernia and scrotal edema due to dialysate leakage through the processus vaginalis: clinical case.
DOI:
https://doi.org/10.25796/bdd.v8i4.87093Keywords:
End-stage Kidney disease, peritoneal dialysis, hernia, scrotal edema, patent processus vaginalisAbstract
Peritoneal dialysis is a therapeutic option for end-stage kidney disease patients that offers a better quality of life Peritoneal dialysis is a treatment option for patients with stage V chronic kidney disease that offers a better quality of life compared to hemodialysis. Abdominal wall hernias and scrotal edema are potential complications of peritoneal dialysis that may require discontinuation of the technique. However, radiological diagnosis and treatment of the hernia allow peritoneal dialysis to be resumed. We report here the case of a 72-year-old patient presenting with unilateral recurrence of an inguinal hernia with scrotal edema after bilateral open repair due to leakage of peritoneal dialysis fluid through a patent processus vaginalis, and we reviewed the existing literature. The literature reports that 4 to 14% of peritoneal dialysis patients develop an abdominal hernia and that dialysate leakage or scrotal edema, which are rarer, are often associated with an indirect inguinal hernia or a persistent patent processus vaginalis. Several risk factors have been identified: age, male gender, obesity, polycystic kidney disease, history of hernia, and high dialysate volumes. The diagnosis is based mainly on peritoneal computed tomography. Management may be conservative, but surgical repair using a tension-free technique, preferably according to Lichtenstein, is recommended in cases of confirmed primary or recurrent hernia. The optimal time to resume peritoneal dialysis remains variable, but is most often between 2 and 6 weeks.
Introduction
Peritoneal dialysis (PD) is a therapeutic option for patients with end-stage kidney disease (ESKD) that offers better dynamism, independence, and quality of life than hemodialysis (HD) 1. Patients usually initiate PD by manually performing dwells, a method known as continuous ambulatory peritoneal dialysis (CAPD). However, PD is associated with complications such as malfunctions of the dialysis catheter (DC), infections (peritonitis, infections of the peritoneal DC, and tunnel and exit site infections), and abdominal wall defects with inguinal hernia (IH) that may present rarely with acute scrotal edema 2. Abdominal wall hernias and scrotal edema are potential complications of PD in adults that may force interruption of the therapy. In contrast to children, in whom inguinoscrotal hernia through a patent processus vaginalis (PPV) is common, such pathology is very rare in adults.
Clinical history
We herein report the case of a 72-year-old man with end-stage kidney disease (ESKD) and a history of type 2 diabetes, arterial hypertension, obesity (BMI>31 kg/m²), hypercholesterolemia, and a history of bilateral IH treated by open Stoppa tension-free mesh hernioplasty (TFMH). A Tenchkoff PD catheter had been placed simultaneously to hernia repair because of advanced chronic kidney disease, with a GFR of 13 ml/min/1.73m² according to the CKD-EPI equation. In the next six months, due to deteriorating renal function with uremic symptoms, the PD catheter was externalized, and PD was initiated after 4 weeks.
Within 48 hours after PD initiation, the patient presented with acute right-sided scrotal edema. CT-peritoneography was performed and revealed the recurrence of a right IH due to leakage of persistent dialysate fluid through a PPV (Figure 1).
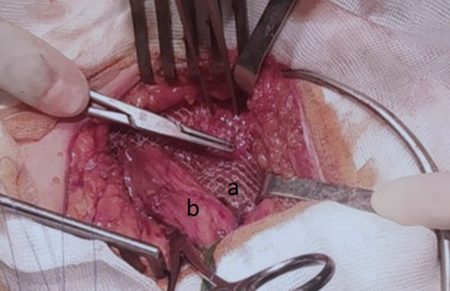
His right IH was treated by open Lichtenstein TFMH (Figure 2), and PD was resumed 4 weeks after the operation. Currently, after 12 months of follow-up, the patient remains recurrence-free while on CAPD due to his preference.
Figure 1.Figure 1. CT-peritoneography with 3D reconstruction showing genital leakage associated with right PPV.
Figure 2.Figure 2. Hernioplasty according to the Lichtenstein technique. a: Polypropylene mesh, b: Spermatic cord
Literature analysis
Abdominal wall hernias are estimated to affect 4% to 14% of PD patients and are commonly caused by chronic high intra-abdominal pressure 3. When symptomatic, they may warrant interrupting PD until the problem is identified and resolved. If surgery is indicated, TFMH is the currently recommended treatment before resuming PD after a variable postoperative delay 23. Unfortunately, undiagnosed IH may manifest primarily after PD initiation or rarely as a recurrence following previous TFMH 3. Our patient experienced the recurrence of right IH through a PPV after bilateral open IH repair using the Stoppa approach 6 months ago. Acute scrotal edema manifested within 48 hours after his first PD session, and PD had to be stopped. To our knowledge, such recurrence in a CAPD-ESKD patient has not been reported yet. The patient was offered open surgical repair with tension-free mesh placement using the Lichtenstein approach and resection of the herniary sac. The postoperative course was uneventful, and PD could be restarted 6 weeks after the surgery; a one-year follow-up found no herniary recurrence or related complications.
PD patients have a high risk of abdominal wall complications such as dialysate leak (5-10%), hernias (10-37%; mostly inguinal and umbilical hernias), or acute scrotal edema (2-4%) 45. Acute scrotal edema is uncommon and often associated with an IH. There are risk factors for ESKD patients that may increase the likelihood of abdominal hernias (elderly males and those with polycystic kidney disease, previous hernia repair, midline incision for PD catheter placement, high BMI, greater residual volume, and prolonged PD duration are at greater risk) 3678. Additionally, the large volumes of fluid injected into the peritoneal cavity during CAPD may increase intra-abdominal pressure 3678 and force the fluid into the genitalia indirectly through an abdominal wall defect, or directly through an IH or PPV, causing scrotal edema 9. This process affects ultrafiltration efficiency and PD 37. In adults, indirect IH is almost always congenital and attributed to a failure of PV closure 1011. A small, indirect IH may unfortunately be missed before PD initiation and become clinically evident 3 to 105 months later 41011. When an IH is diagnosed before PD initiation, surgical treatment should be considered to prevent complications (decreased ultrafiltration efficiency, discomfort, recurrent peritonitis, incarceration, strangulation, necrosis, and perforation), particularly for irreducible hernias, considering that other hernias, such as reducible umbilical hernia, can still be managed conservatively in up to 71.42% of cases 347.
When indirect IH is suspected in an ESKD patient with PD and scrotal edema, CTperitoneography is considered the reference imaging study, considering its high detection rate 3. However, factors such as the risks associated with radiation exposure and allergy to contrast product may indicate other imaging studies such as abdominal ultrasound, peritoneal scintigraphy, or peritoneal magnetic resonance imaging 1213. Diagnostic laparoscopy may also help to confirm the diagnosis by excluding the possibility of a contralateral IH and a concomitant open repair with mesh 5. As of now, there is no consensus on the management of IH with scrotal edema in ESKD patients. Sometimes, a small indirect IH due to PPV can be treated conservatively with a 1-to-3week rest from PD or a temporary shift to HD or modified PD to decrease the volume of peritoneal fluid and intra-abdominal pressure 14. If surgery is indicated, the reference is open TFMH using the Lichtenstein technique 315. However, recurrence occurs up to 60% of the time. Other TFMH techniques, such as an anterior, posterior (Stoppa technique), or laparoscopic approach, have been shown to have a low recurrence rate but a steeper learning curve 16. Hernioplasty is usually performed simultaneously with the placement of the PD catheter. In the literature, a posterior open approach for IH repair (the Stoppa technique) is indicated for patients aged over 50 with bilateral IH; this approach results in a low recurrence rate of 0.7% 1718. However, as the mesh retracts by up to 20% over 6 months, an insufficiently large mesh may trigger recurrence 19. In a case series involving 14 patients, the Lichtenstein procedure with sac excision was associated with a good outcome. No PD-related complications were observed, and no recurrence was observed during a follow-up after about 3 and a half years 20. In our patient, the right IH reappeared after Stoppa hernioplasty and was treated by TFMH using the Lichtenstein approach without recurrence. Postoperatively, increased intra-abdominal pressure and chronic renal failure may impair tissue healing, and the optimal timing for PD reinitiation remains undefined 34.
PD is usually restarted at normal volumes within 2-4 weeks; during this interval, lowvolume PD is used with frequent exchanges, which are gradually increased to regain the preoperative CAPD regimen 34.
Despite some conflicting data on the association between intraperitoneal volume infusion and intraperitoneal pressure 21, automated peritoneal dialysis (APD) using smallervolume dwells while the patient is recumbent during the night is an attractive approach in these situations. Indeed, supine exchanges have been associated with decreased intraabdominal pressure per volume of dialysate (as intraperitoneal pressure parallels intraperitoneal volume) with similar efficacy to other techniques 22.
Thus, APD has been used effectively in place of CAPD in ESKD patients who develop abdominal wall hernias 34714. Interestingly, laparoscopic transabdominal preperitoneal (TAPP) IH repair may decrease morbidity and the recurrence rate compared to open surgery and PD resumption after 7 days 23. In our case, PD was restarted with normal volumes after 6 weeks when the surgical wound had completely healed. Despite our short follow-up interval of 1 year, the patient remains recurrence-free, in line with the low recurrence rate reported in the literature 3.
Conclusion
In conclusion, TFMH should always be proposed before PD in ESKD patients when IH is diagnosed. The recurrence rate of IH after Stoppa bilateral TFMH is as high as 1.7%, and factors such as the failure to diagnose occult PPV before the initiation of PD may trigger this recurrence 19. Scrotal edema arising after PD initiation suggests the existence of an indirect IH and potentially a PPV. Different imaging studies may help with the diagnosis depending on the context, but a CT-peritoneogram is still considered the reference. The surgical correction of the primary or recurring IH should not be delayed, allowing PD reinitiation as soon as possible.
Authors’ Contributions
VC, MT, MAL, MEK, FM and JN contributed to the clinical management of the patient and data collection. VC and MT drafted the manuscript. MAL, MED, FM and JN participated in critical revision and improvement of the content. JN did the supervision. All authors approved the final version of the manuscript and agree to take responsibility for it
Ethical Considerations
No information that could identify the patient has been disclosed.
Patient Consent
Informed consent of the infant's parents was obtained for the publication of this case report.
Data Availabilité Statement
Not applicable
Funding
The authors did not receive any funding for the report
Conflicts of Interest
The authors declare no conflicts of interest
ORCID iDs
Maximze Taghavi: https://orcid.org/0000-0003-1442-9716
Moncef Al Barajraji: https://orcid.org/0009-0005-3187-5736
References
- Li P.K., Chow K.M.. Peritoneal dialysis-first policy made successful: perspectives and actions. Am J Kidney Dis. 2013; 62(5):993-1005. DOI
- Esagian S.M., Spinos D., Vasilopoulou A., Syrigos N., Bishawi M., Lehrich R.W., Middleton J.P., Suhocki P.V., Pappas T.N., Economopoulos K.P.. Influence of peritoneal dialysis catheter type on complications and long-term outcomes: an updated systematic review and meta-analysis. J Nephrol. 2021; 34(6):1973-1987. DOI
- Chi Q., Shi Z., Zhang Z., Lin C., Liu G., Weng S.. Inguinal hernias in patients on continuous ambulatory peritoneal dialysis: is tension-free mesh repair feasible?. BMC Surg. 2020; 20(1)DOI
- Girimaji N., Sunnesh A., Nagalakshmi T., Bethasaida Manuel M., Reddy Vutukuru V., Rapur R., Vishnubhotla S.. Prevalence and outcome of abdominal wall hernia in patients with end-stage renal disease on peritoneal dialysis. Ther Apher Dial. 2023; 27(2):320-327. DOI
- Haggerty S.P., Jorge J.M.. Laparoscopy to evaluate scrotal edema during peritoneal dialysis. JSLS. 2013; 17(3):429-432. DOI
- García-Ureña M.A., Rodríguez C.R., Vega Ruiz V., Carnero Hernández F.J., Fernández-Ruiz E., Vazquez Gallego J.M., Velasco García M.. Prevalence and management of hernias in peritoneal dialysis patients. Perit Dial Int. 2006.
- Balda S., Power A., Papalois V., Brown E.. Impact of hernias on peritoneal dialysis technique survival and residual renal function. Perit Dial Int. 2013; 33(6):629-634. DOI
- Yang S.F., Liu C.J., Yang W.C., Chang C.F., Yang C.Y., Li S.Y., Lin C.C.. The risk factors and the impact of hernia development on technique survival in peritoneal dialysis patients: a population-based cohort study. Perit Dial Int. 2015; 35(3):351-359. DOI
- Davidson P.G., Usal H., Fiorillo M.A., Maniscalco A.. The importance of peritoneal imaging in the workup of genital edema in patients on continuous ambulatory peritoneal dialysis. Mt Sinai J Med. 1999.
- Read R.C.. British contributions to modern herniology of the groin. Hernia. 2005; 9(1):6-11. DOI
- Banshodani M., Kawanishi H., Moriishi M., Shintaku S., Hashimoto S., Nishihara M.. Inguinal hernia in hemodialysis versus peritoneal dialysis patients: a case-control study. Ren Replace Ther. 2016; 2(1):1-5. DOI
- Tokmak H., Mudun A., Türkmen C., Sanli Y., Cantez S., Bozfakioğlu S.. The role of peritoneal scintigraphy in the detection of continuous ambulatory peritoneal dialysis complications. Ren Fail. 2006; 28(8):709-713. DOI
- Prokesch R.W., Schima W., Schober E., Vychytil A., Fabrizii V., Bader T.R.. Complications of continuous ambulatory peritoneal dialysis: findings on MR peritoneography. Am J Roentgenol. 2000; 174(4):987-991. DOI
- Al-Wadani H., Alqahtani A.A., Al-Dossari N., Alsawad A., Al-Atiqu M., Saad I., Al-Hwiesh A.K.. Conservative treatment of processus vaginalis hernia in two peritoneal dialysis patients. Saudi J Kidney Dis Transplant. 2010.
- Luk Y., Li J.Y.Y., Law T.T., Ng L., Wong K.Y.. Tension-free mesh repair of inguinal hernia in patients on continuous ambulatory peritoneal dialysis. Perit Dial Int. 2020; 40(1):62-66. DOI
- Pereira C., Rai R.. Open Lichtenstein hernioplasty versus laparoscopic transabdominal preperitoneal mesh repair: the pain factor. Cureus. 2021; 2021;13(9):e18282DOI
- Stoppa R.E., Warlaumont C.R., Verhaeghe P.J., Romero E.R., M’Balla-N’Di C.J.. Prosthetic repair in the treatment of groin hernias. Int Surg. 1986.
- Solorzano C.C., Minter R.M., Childers T.C., Kilkenny J.W., Vauthey J.N.. Prospective evaluation of the giant prosthetic reinforcement of the visceral sac for recurrent and complex bilateral inguinal hernias. Am J Surg. 1999; 1999;177(1):19-22DOI
- Fernández-Lobato R., Tartas-Ruiz A., Jiménez-Miramón F.J., Marín-Lucas F.J., Adana-Belbel J.C., Esteban M.L.. Stoppa procedure in bilateral inguinal hernia. Hernia. 2006; 10(2):179-183. DOI
- Iyasu Y., Ogata N., Matsuda S., Kusanagi H.. Safety of hernia sac resection in inguinal herniorrhaphy for patients on peritoneal dialysis: a case series. Hernia. 2024. DOI
- Leung K.C., Mahony S., Brown E.A., Corbett R.W.. Factors affecting intraperitoneal pressure (IPP) and its prognostic value in predicting leak risk and gastrointestinal symptoms in adult peritoneal dialysis patients: a systematic review and meta-analysis. J Nephrol. 2024. DOI
- Enoch C., Aslam N., Piraino B.. Intra-abdominal pressure, peritoneal dialysis exchange volume, and tolerance in APD. Semin Dial. 2002; v-Dec;15(6):403-6DOI
- Cui C., Zhang L., Luan L., Liu Q., Cheng Y., Li B.. Laparoscopic techniques in treatment of inguinal hernia in patients with peritoneal dialysis: experiences from 15 cases. J Laparoendosc Adv Surg Tech - A. 2023; 2023;33(8):738-742DOI
References
Li PK, Chow KM. Peritoneal dialysis-first policy made successful: perspectives and actions. Am J Kidney Dis. 2013;62(5):993-1005. doi: https://doi.org/10.1053/j.ajkd.2013.03.038
Esagian SM, Spinos D, Vasilopoulou A, Syrigos N, Bishawi M, Lehrich RW, Middleton JP, Suhocki PV, Pappas TN, Economopoulos KP. Influence of peritoneal dialysis catheter type on complications and long-term outcomes: an updated systematic review and meta-analysis. J Nephrol. 2021;34(6):1973–1987. doi: https://doi.org/10.1007/s40620-021-01016-y
Chi Q, Shi Z, Zhang Z, Lin C, Liu G, Weng S. Inguinal hernias in patients on continuous ambulatory peritoneal dialysis: is tension-free mesh repair feasible? BMC Surg. 2020;20(1):310. doi: https://doi.org/10.1186/s12893-020-00979-2
Girimaji N, Sunnesh A, Nagalakshmi T, Bethasaida Manuel M, Reddy Vutukuru V, Rapur R, Vishnubhotla S. Prevalence and outcome of abdominal wall hernia in patients with end-stage renal disease on peritoneal dialysis. Ther Apher Dial. 2023;27(2):320-327. doi: https://doi.org/10.1111/1744-9987.13917
Haggerty SP, Jorge JM. Laparoscopy to evaluate scrotal edema during peritoneal dialysis. JSLS. 2013;17(3):429-432. doi: https://doi.org/10.4293/108680813x13693422521674
García-Ureña MA, Rodríguez CR, Vega Ruiz V, Carnero Hernández FJ, Fernández-Ruiz E, Vazquez Gallego JM, Velasco García M. (2006). Prevalence and management of hernias in peritoneal dialysis patients. Perit Dial Int. 2006 Mar-Apr;26(2):198-202.
Balda S, Power A, Papalois V, Brown E. Impact of hernias on peritoneal dialysis technique survival and residual renal function. Perit Dial Int. 2013;33(6):629-634. doi: https://doi.org/10.3747/pdi.2012.00255
Yang SF, Liu CJ, Yang WC, Chang CF, Yang CY, Li SY, Lin CC. The risk factors and the impact of hernia development on technique survival in peritoneal dialysis patients: a population-based cohort study. Perit Dial Int. 2015;35(3):351-359. doi: https://doi.org/10.3747/pdi.2013.00139
Davidson PG, Usal H, Fiorillo MA, Maniscalco A. The importance of peritoneal imaging in the workup of genital edema in patients on continuous ambulatory peritoneal dialysis. Mt Sinai J Med. 1999 Mar;66(2):125-127.
Read RC. British contributions to modern herniology of the groin. Hernia. 2005;9(1):6-11. doi: https://doi.org/10.1007/s10029-004-0285-7
Banshodani M, Kawanishi H, Moriishi M, Shintaku S, Hashimoto S, Nishihara M. Inguinal hernia in hemodialysis versus peritoneal dialysis patients: a case-control study. Ren Replace Ther. 2016;2(1):1-5. doi: https://doi.org/10.1186/s41100-016-0035-1
Tokmak H, Mudun A, Türkmen C, Sanli Y, Cantez S, Bozfakioğlu S. The role of peritoneal scintigraphy in the detection of continuous ambulatory peritoneal dialysis complications. Ren Fail. 2006;28(8):709-713. doi: https://doi.org/10.1080/08860220600925396
Prokesch RW, Schima W, Schober E, Vychytil A, Fabrizii V, Bader TR. Complications of continuous ambulatory peritoneal dialysis: findings on MR peritoneography. Am J Roentgenol. 2000;174(4):987-991. doi: https://doi.org/10.2214/ajr.174.4.1740987
Al-Wadani H, Alqahtani AA, Al-Dossari N, Alsawad A, Al-Atiqu M, Saad I, Al-Hwiesh AK. Conservative treatment of processus vaginalis hernia in two peritoneal dialysis patients. Saudi J Kidney Dis Transplant. 2010 May;21(3):507-10.
Luk Y, Li JYY, Law TT, Ng L, Wong KY. Tension-free mesh repair of inguinal hernia in patients on continuous ambulatory peritoneal dialysis. Perit Dial Int. 2020;40(1):62-66. doi: https://doi.org/10.1177/0896860819879596
Pereira C, Rai R. (2021). Open Lichtenstein hernioplasty versus laparoscopic transabdominal preperitoneal mesh repair: the pain factor. Cureus. 2021;13(9):e18282. doi: https://doi.org/10.7759/cureus.18282
Stoppa RE, Warlaumont CR, Verhaeghe PJ, Romero ER, M’Balla-N’Di CJ. Prosthetic repair in the treatment of groin hernias. Int Surg. 1986 Jul-Sep;71(3):154-8.
Solorzano CC, Minter RM, Childers TC, Kilkenny JW, Vauthey JN. (1999). Prospective evaluation of the giant prosthetic reinforcement of the visceral sac for recurrent and complex bilateral inguinal hernias. Am J Surg. 1999;177(1):19-22. doi: https://doi.org/10.1016/s0002-9610(98)00292-x
Fernández-Lobato R, Tartas-Ruiz A, Jiménez-Miramón FJ, Marín-Lucas FJ, de Adana-Belbel JC, Esteban ML. Stoppa procedure in bilateral inguinal hernia. Hernia. 2006;10(2):179-183. doi: https://doi.org/10.1007/s10029-005-0061-3
Iyasu Y, Ogata N, Matsuda S, Kusanagi H. Safety of hernia sac resection in inguinal herniorrhaphy for patients on peritoneal dialysis: a case series. Hernia. 2024 Dec;28(6):2411-2414. doi: https://doi.org/10.1007/s10029-024-03166-x
Leung KC, Mahony S, Brown EA, Corbett RW. Factors affecting intraperitoneal pressure (IPP) and its prognostic value in predicting leak risk and gastrointestinal symptoms in adult peritoneal dialysis patients: a systematic review and meta-analysis. J Nephrol. 2024 Sep;37(7):1767-1777. doi: https://doi.org/10.1007/s40620-024-02091-7
Enoch C, Aslam N, Piraino B. Intra-abdominal pressure, peritoneal dialysis exchange volume, and tolerance in APD. Semin Dial. 2002 Nov-Dec;15(6):403-6. doi: https://doi.org/10.1046/j.1525-139x.2002.00100.x
Cui C, Zhang L, Luan L, Liu Q, Cheng Y, Li B. (2023). Laparoscopic techniques in treatment of inguinal hernia in patients with peritoneal dialysis: experiences from 15 cases. J Laparoendosc Adv Surg Tech - A. 2023;33(8):738-742. doi: https://doi.org/10.1089/lap.2023.0088
Downloads
Submitted
Accepted
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Victor Calderon, Maxime Taghavi, Moncef Al Barajraji, Michael El Khoury, Freddy Mboti, Johanna Noels

This work is licensed under a Creative Commons Attribution 4.0 International License.






